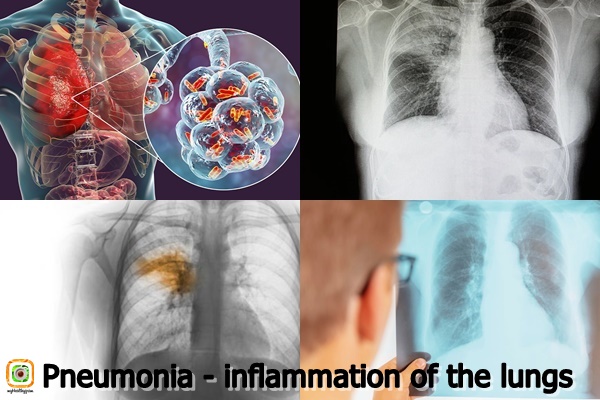
The lungs are air-filled “spongy” organs whose primary function is gas exchange, or the delivery of oxygen from the atmosphere to the bloodstream and the release of carbon dioxide from the blood into the atmosphere. The alveoli, which are small structures in the shape of bubbles that are filled with air in a healthy person, play a key part in the gas exchange process. Pneumonia causes the alveoli to fill with pus and fluid, interfering with the gas exchange mechanism.
Pneumonia is an inflammation of the lungs, a health condition that indicates urgent treatment because it can have fatal consequences, especially in the younger population. Namely, pneumonia is the leading cause of death in children up to 5 years of age.
Causes and risk factors
The human body has a number of defense systems that guard against infectious particles and prevent pneumonia (sneezing, coughing, specific cell structure of the respiratory system, immune system). An infection arises when pathogenic germs outnumber the body’s defense mechanisms.
Pneumonia can be caused by bacteria, viruses, rickettsiae, mycoplasmas, parasites, fungus, and other microbes. Streptococcus pneumoniae, Haemophilus influenzae, Mycoplasma pneumoniae, Legionella pneumophyla, Chlamydia pneumoniae, Influenza virus, CMV (cytomegalovirus), and other bacteria are among the most prevalent.
Pneumonia can occur in any individual, but there are certain categories of people who are more vulnerable such as:
- People who have a chronic illness (asthma, COPD, diabetes, cardiovascular disease, etc.);
- Persons over 65 years of age;
- Children up to 2 years of age;
- Smokers;
- People who due to their profession are often exposed to chemicals, dust, toxic gases, etc .;
- People with reduced immunity (people infected with HIV);
- Persons who are hospitalized, especially in intensive care.
How is it transmitted?
The entry of pathogenic microorganisms into the lungs can be through:
- Intake of microorganisms from the oropharynx. Aspiration of pulmonary pathogens is the most common mechanism for pneumonia.
- Inhalation of infectious aerosols. These are particles smaller than 3-5 microns that contain microbes. These infectious aerosols are very small, so they can penetrate deep into the airways and cause infection. Just one infectious card may be enough to cause inflammation.
- Infection spreads through the bloodstream. In drug users, patients with venous catheters, patients with endocarditis, and others, harmful bacteria in the lungs are spread through the blood.
- Infection acquired by knife wounds in the lungs or during some medical procedures. Pneumonia can be caused by medical procedures such as tracheal intubation and traumatic lung injury.
- Infection spreads from surrounding tissues. Direct infection transmission and pneumonia may occur if an inflammatory focus is present on organs and organ structures physically adjacent to the lungs.
Symptoms and signs
Depending on the symptoms and signs, we distinguish two clinical syndromes of pneumonia: typical and atypical, although recent research shows that no sharp line can be drawn between the two clinical forms.
Typical pneumonia
In this type of pneumonia the symptoms appear suddenly, for a short period of time. The clinical picture usually includes:
- Fever;
- Elevated body temperature;
- Chest pain that is accentuated by coughing;
- Productive cough with whitish, yellowish or greenish cough;
- Fatigue and malaise;
- Feeling short of breath.
Atypical pneumonia
Unlike the previous one, the clinical picture in atypical pneumonia develops gradually. The following symptoms and signs are characteristic:
- Cough usually without or with a small amount of sputum;
- Headache;
- Subfebrile body temperature or slightly elevated;
- Fatigue and malaise;
- Sore throat;
- Nausea and vomiting;
- Muscle pain.
Diagnose
In order to diagnose pneumonia, the doctor takes a detailed medical history and performs a complete physical examination. Additional tests such as:
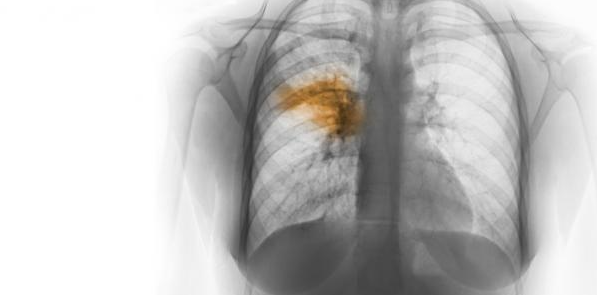
- Lung X-ray – Lung X-ray allows confirmation of the presence of infection and localization of the inflammatory process. Additionally, if therapy has already been given, this diagnostic procedure can monitor whether there is a therapeutic response.
- Sputum examination – The secretion from the lower airways acquired during vigorous coughing is sent to a microbiological examination to determine the cause of pneumonia. Unfortunately, potentially harmful microorganisms that colonize the upper airways frequently contaminate sputum, limiting diagnostic specificity.
- Transthoracic lung puncture – A sample is collected from the location of the pulmonary inflammatory process with the use of a fine needle for further testing.
- Bronchoscopy – With the help of a fiberoscope, direct visualization of the airways and obtaining secretions from the lower airways in seriously ill patients is enabled.
- Blood culture – A sample of venous blood is obtained for microbiological testing. Blood cultures that are positive can help determine the etiology of pneumonia.
- Serological tests – Antibody titers for IgM and IgG can aid in diagnosis.
Treatment and prevention
Antimicrobial therapy should be started immediately, as this is a serious illness. If the cause of the infection is confirmed, specific therapy is given. This means that in the case of bacterial pneumonia caused by Streptococcus pneumoniae, the doctor prescribes antibiotic therapy (Co – amoxiclav, trimethoprim-sulfamethoxazole, Erythromycin, Cefuroxime, Doxycycline, Ciprofloxacin, etc.) to which the specific bacterium is.
If necessary, antipyretics may be taken to reduce fever and cough medicines.
You can try some of the natural remedies at home if you have a sore throat and a persistent cough.
To fight pneumonia faster, drink enough of fluids and get plenty of rest, in addition to following your doctor’s advise and undergoing prescribed therapy on a regular basis.